
 Indications for insulin usage:
Indications for insulin usage:
- When oral medicines fail to control the sugar in maximum doses
- when there are complications to the eyes, kidney or heart,
- when the sugars are very high,
- when there is pregnancy associated with diabetes,
- when intolerant to oral medicines ,
- when diagnosed with latent auto immune diabetes of adults
- when being planned for surgery.
- If diagnosed with type 1 diabetes.
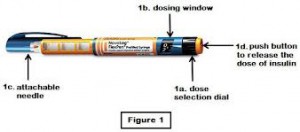
Insulin preparation: There are 3 main types of insulin based on duration of action- short acting, intermediate acting and long acting. • Short acting insulin acts for a short time and peaks fast. This is why this has to be administered with the main meals at least three times a day. • Intermediate acting insulin acts for close to 10 hours and so needs twice daily dosing • The long acting insulin can last for 16-24 hours and thus, needs one or two shots a day • There are premix insulin which comprise short and intermediate acting insulin in one. • Ultra short acting and ultra long acting insulin preparations are now available. • Non injection forms of insulin are now becoming available- studies are on. Nasal, inhaled forms, patches, pills, oral sprays are all forms being researched into to avoid the needle prick. The doses of insulin are usually tailored by the doctor or nurse initially and then adjusted by the patient depending on the sugar reading. Insulin delivery devices are now- a days by pen devices or by continuous subcutaneous devices. The old method of using a vial and syringe is still present. Insulin can be safely administered if used sensibly. Store the insulin in fridges ( not in the freezer) or in a cool room, lightly shake the pen before use if pre mix insulin and roll the insulin pen between the palms of the hand to prevent injecting cold insulin and inject at different sites each time. The needles are to ideally thrown after each injection( though some can use up to 3 injections with a needle) . Sites for injecting: 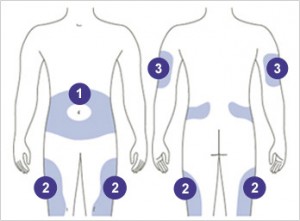 • The thighs on inner side, the outer side and front side are the most preferred sites. • The abdomen wall can be used- but remember not to inject just around the belly button ( umbilicus) inject any place on the flanks more than two finger breaths on either side of the umbilicus. • The arms are not commonly used in adults. • The buttocks and back are used for small children
• The thighs on inner side, the outer side and front side are the most preferred sites. • The abdomen wall can be used- but remember not to inject just around the belly button ( umbilicus) inject any place on the flanks more than two finger breaths on either side of the umbilicus. • The arms are not commonly used in adults. • The buttocks and back are used for small children  How to inject: • Have the needles changed before injecting • Roll the insulin between the palms of the hands if insulin is cold. • Select the site for injection. It is not mandatory to wipe the area with a spirit wipe. However, if you do, make sure the alcohol or spirit dries out before injecting. • Feel for any thickening or induration. If present, avoid injecting into that site. • If skin is dark at that site avoid injecting there. • Do not inject into dilated veins on the thigh, if present. • Dial the required dose. • There are people who pinch a fold of skin before injecting. It is not necessary to. • Plunge the needle vertically into the site ( perpendicular to skin and not at an angle). Needles are fine and almost painless • Depress the plunger down. The meter will return to zero. • Count to five slowly and remove the pen. • It is common to see a drop of blood after removing the needle. • There is no need for a vigorous massage as is done after deep intramuscular injections. • Do not inject soon before or after an exercise regime. • Rapid acting ( short acting) insulin can be injected in the abdominal wall. The absorption from the thighs is ideal for intermediate and long acting insulin as the absorption is not so fast. The absorption of insulin is slowest if injected in the buttocks. The arm is not ideal for self injection. • The pen device has a spring device which can get worn out over a period of time, maybe after an year or two. Change the delivery system when this happens. The needles after use are to be discarded in a proper manner after putting them in a sharps container. There are places around the world where the used needles are sold again in a fresh pack thus helping spread of disease such as AIDS, Hepatitis B and Hepatitis C. Side effects of insulin: • Hypoglycemia- low sugar • Allergy to the preservative or type of insulin( this is quite rare these days with the advent of purified and human varieties of insulin) • Weight gain • Thickening of the subcutaneous tissue at injection site • Neuropathy– sometimes insulin can cause nerve pain which can be very depressing. Being started on insulin does not mean the end of the road. It is used by the doctor when the sugar levels are very high to bring I down, or when you are undergoing an operation or when you are pregnant or when you have complications affecting the eyes, kidney or heart. It does not mean that insulin once started remains so for the rest of your life. There are needless insulin delivery systems which are present elsewhere. There are other insulin routes available which had been researched, but fell out of favor due to the less efficiency. . While traveling long distances, use a temperature controlled pouch or ice box for keeping the insulin at a cool temperature. If you party, take a small dose before the party, have a snack before you leave, and have the rapid acting insulin after the dinner .Meet your doctor for advice on the dose. Alcohol intake can cause a delayed hypoglycemia(low sugar) The three main insulin delivery options are a pen, syringe, or pump. There are also a few newer insulin delivery systems, including the jet injector. Here are the pros and cons of each insulin delivery method to help you get started. Most of the insurance companies do not approve of these delivery systems which are new and innovative. The pen delivery system is, of course, approved and effective. Pen, Pump, or Syringe? Here’s a rundown of the three different insulin delivery systems, how they work, and their pros and cons. Insulin Syringe You use an insulin syringe to inject insulin into your body with a very fine needle. Pros: • Flexibility. You can choose from many different brands and types of syringes, and you can use them with just about any kind of insulin. • Cost savings. These work more economical than the latest medicines which could be very costly. • People with very regular schedules and consistent meal patterns can do well using this method. Cons: • Time. You have to be meticulous in loading the syringe, remember to warm the insulin if cold , by rolling the cartridge in the palm three or four times. Before injecting you need to check there is no air bubble, attach the needle, and draw the correct dose of insulin into the syringe. • Dosing mistakes. Sometimes error while loading the dose can lead to problems. Insulin Pen An insulin pen works much like a syringe, but it looks like the type of pen you use to write. Insulin pens come in disposable and reusable versions. • Disposable pens come pre-filled with insulin. • Reusable pens use a cartridge filled with insulin. Pros: • Ease and convenience. Pens are convenient to carry about unlike the insulin which ( and still is) comes in bottles.. To use an insulin pen, you just dial up the insulin dose on the pen. Then you press a plunger at one end to inject the insulin through a needle at the other end. • Memory storage. Insulin pens have a handy memory feature that will remind you how much insulin you took, and when you took it. Cons: • Expense. The disposable pens are costly and the ones which could be reused are more economical. However, the reusable ones may have to be changed once in a year or two as the dose dialer spring may become faulty. • Lack of options. Some types of insulin are not available in pen form. Insulin Pump An insulin pump is a device that’s about the same size as a pager. You wear it on your belt or in a pocket, and it delivers a steady stream of rapid acting insulin to your body 24 hours a day through a needle attached to a flexible plastic tube. Whenever you eat, you press a button on the pump to give yourself an extra boost of insulin, called a bolus. The pump is an option for people with type 1 diabetes who have not reached their target blood sugar level using other delivery methods. It’s also a good option for people with diabetes that have very active lifestyles. It’s not clear whether people with type 2 diabetes benefit from using a pump. However among those with type 2 diabetes, who have failed to achieve good sugar control with maximum doses and have to take multiple doses of insulin instead, this is a convenient option. Pros: • Steady insulin release. The pump releases insulin as if mimicking the pancreas. The dose of insulin used will be quite less as it will be delivering tiny doses at pre fixed times. Only short acting insulin is used in this. Pumps are so efficient that you can use less insulin than you would with a syringe or pen. • Ease of use. You’ll no longer have to give yourself injections of insulin throughout the day–the pump will do it for you automatically. You can also eat whenever you choose. • Better blood sugar control. Because it delivers insulin steadily like your pancreas, the pump helps prevent blood sugar swings. • Ease of monitoring. Your pump can communicate with your glucose monitoring system so you can track your blood sugar over time and make changes to your routine as needed. Cons: • Constant wear. You’re going to be attached to this pump nearly all of the time — even when you sleep. • Risks. You need to be very careful about changing the needle every couple of days because there is a slight risk for infection. You also have to monitor your blood sugar levels, because you may be more likely to have a drop in blood sugar (hypoglycemia) with the pump than with a syringe or pen. If the catheter slips out or the pump fails, you might not get the insulin you need and over time your sugars can increase and you could develop a dangerous complication called diabetic ketoacidosis. • Cost. Pumps are costly and so also are the infusion tubing and reservoir. Some of the new ones come with inbuilt sensors as well which are costly. Insurance companies do not approve of this usually. • The infusion tubing and reservoir have to changed once every three days • Sometimes the tubing gets kinked without delivering the insulin which could cause problems • One has to feed in the carbohydrate consumption at the start to prime the pump. • The insulin will not be delivered if there is air in the tubing or if the insulin remaining in the cartridge is very low. Jet Injector Jet injectors don’t have a needle. Instead, they use very high pressure to push a fine spray of insulin through the pores in your skin. Pros: • Needle-free. If you hate needles, a jet injector is an alternative to the insulin syringe or pen. Cons: • Pain. Though needle less, they can cause more pain in some of those with sensitive skin as the insulin is driven inside the body by sheer force. You have a high concentration of nerves close to the surface of your skin. Trying to push insulin through the skin can hurt more than injecting — especially considering how thin needles are. • Uneven insulin delivery. Because they send insulin into the body through the pores, jet injectors may not always deliver an accurate dose. Other options include an insulin patch. Work closely with your doctor to choose the option that best fits your budget, health needs, and lifestyle. Not all the above are available here in Oman. Afreeza is a powder form of insulin which is an ultra rapid acting insulin. The powder is used by an inhaler called the Dreamboat inhaler. Peak levels are reported in 12-14 minutes of inhalation. This is especially beneficial for those with type 1 diabetes who are dependent on insulin for life and also for those with type 2 who become insulin dependent with failure of the pancreas. Close to 5300 patients have been studied in trails across the world and the results so far are promising, but needs further time to be found effective. This has been found to reduce the post meal sugar levels, fasting levels, have less incidence of hypoglycemia( term used for low sugar levels) , reduced weight gain as when compared to rapid acting insulin. However, this may need to be combined with long acting insulin or with oral medicines as the case may be for a better effect. The side effect so far noted has been a non productive cough ( dry cough) Degludec insulin is a new ultra long acting insulin which is still on research programs to test its efficacy. Though it is being marketed for injection once in 3 days or once a week ( which sounds like sweet music) , the effects of the insulin wear off after a day or two. Which means it is still better to have the shots of insulin daily for better control. The sugar control and episodes of low sugar have not shown any improvement over the insulin preparations available in the market today. Continuous glucose monitoring
How to inject: • Have the needles changed before injecting • Roll the insulin between the palms of the hands if insulin is cold. • Select the site for injection. It is not mandatory to wipe the area with a spirit wipe. However, if you do, make sure the alcohol or spirit dries out before injecting. • Feel for any thickening or induration. If present, avoid injecting into that site. • If skin is dark at that site avoid injecting there. • Do not inject into dilated veins on the thigh, if present. • Dial the required dose. • There are people who pinch a fold of skin before injecting. It is not necessary to. • Plunge the needle vertically into the site ( perpendicular to skin and not at an angle). Needles are fine and almost painless • Depress the plunger down. The meter will return to zero. • Count to five slowly and remove the pen. • It is common to see a drop of blood after removing the needle. • There is no need for a vigorous massage as is done after deep intramuscular injections. • Do not inject soon before or after an exercise regime. • Rapid acting ( short acting) insulin can be injected in the abdominal wall. The absorption from the thighs is ideal for intermediate and long acting insulin as the absorption is not so fast. The absorption of insulin is slowest if injected in the buttocks. The arm is not ideal for self injection. • The pen device has a spring device which can get worn out over a period of time, maybe after an year or two. Change the delivery system when this happens. The needles after use are to be discarded in a proper manner after putting them in a sharps container. There are places around the world where the used needles are sold again in a fresh pack thus helping spread of disease such as AIDS, Hepatitis B and Hepatitis C. Side effects of insulin: • Hypoglycemia- low sugar • Allergy to the preservative or type of insulin( this is quite rare these days with the advent of purified and human varieties of insulin) • Weight gain • Thickening of the subcutaneous tissue at injection site • Neuropathy– sometimes insulin can cause nerve pain which can be very depressing. Being started on insulin does not mean the end of the road. It is used by the doctor when the sugar levels are very high to bring I down, or when you are undergoing an operation or when you are pregnant or when you have complications affecting the eyes, kidney or heart. It does not mean that insulin once started remains so for the rest of your life. There are needless insulin delivery systems which are present elsewhere. There are other insulin routes available which had been researched, but fell out of favor due to the less efficiency. . While traveling long distances, use a temperature controlled pouch or ice box for keeping the insulin at a cool temperature. If you party, take a small dose before the party, have a snack before you leave, and have the rapid acting insulin after the dinner .Meet your doctor for advice on the dose. Alcohol intake can cause a delayed hypoglycemia(low sugar) The three main insulin delivery options are a pen, syringe, or pump. There are also a few newer insulin delivery systems, including the jet injector. Here are the pros and cons of each insulin delivery method to help you get started. Most of the insurance companies do not approve of these delivery systems which are new and innovative. The pen delivery system is, of course, approved and effective. Pen, Pump, or Syringe? Here’s a rundown of the three different insulin delivery systems, how they work, and their pros and cons. Insulin Syringe You use an insulin syringe to inject insulin into your body with a very fine needle. Pros: • Flexibility. You can choose from many different brands and types of syringes, and you can use them with just about any kind of insulin. • Cost savings. These work more economical than the latest medicines which could be very costly. • People with very regular schedules and consistent meal patterns can do well using this method. Cons: • Time. You have to be meticulous in loading the syringe, remember to warm the insulin if cold , by rolling the cartridge in the palm three or four times. Before injecting you need to check there is no air bubble, attach the needle, and draw the correct dose of insulin into the syringe. • Dosing mistakes. Sometimes error while loading the dose can lead to problems. Insulin Pen An insulin pen works much like a syringe, but it looks like the type of pen you use to write. Insulin pens come in disposable and reusable versions. • Disposable pens come pre-filled with insulin. • Reusable pens use a cartridge filled with insulin. Pros: • Ease and convenience. Pens are convenient to carry about unlike the insulin which ( and still is) comes in bottles.. To use an insulin pen, you just dial up the insulin dose on the pen. Then you press a plunger at one end to inject the insulin through a needle at the other end. • Memory storage. Insulin pens have a handy memory feature that will remind you how much insulin you took, and when you took it. Cons: • Expense. The disposable pens are costly and the ones which could be reused are more economical. However, the reusable ones may have to be changed once in a year or two as the dose dialer spring may become faulty. • Lack of options. Some types of insulin are not available in pen form. Insulin Pump An insulin pump is a device that’s about the same size as a pager. You wear it on your belt or in a pocket, and it delivers a steady stream of rapid acting insulin to your body 24 hours a day through a needle attached to a flexible plastic tube. Whenever you eat, you press a button on the pump to give yourself an extra boost of insulin, called a bolus. The pump is an option for people with type 1 diabetes who have not reached their target blood sugar level using other delivery methods. It’s also a good option for people with diabetes that have very active lifestyles. It’s not clear whether people with type 2 diabetes benefit from using a pump. However among those with type 2 diabetes, who have failed to achieve good sugar control with maximum doses and have to take multiple doses of insulin instead, this is a convenient option. Pros: • Steady insulin release. The pump releases insulin as if mimicking the pancreas. The dose of insulin used will be quite less as it will be delivering tiny doses at pre fixed times. Only short acting insulin is used in this. Pumps are so efficient that you can use less insulin than you would with a syringe or pen. • Ease of use. You’ll no longer have to give yourself injections of insulin throughout the day–the pump will do it for you automatically. You can also eat whenever you choose. • Better blood sugar control. Because it delivers insulin steadily like your pancreas, the pump helps prevent blood sugar swings. • Ease of monitoring. Your pump can communicate with your glucose monitoring system so you can track your blood sugar over time and make changes to your routine as needed. Cons: • Constant wear. You’re going to be attached to this pump nearly all of the time — even when you sleep. • Risks. You need to be very careful about changing the needle every couple of days because there is a slight risk for infection. You also have to monitor your blood sugar levels, because you may be more likely to have a drop in blood sugar (hypoglycemia) with the pump than with a syringe or pen. If the catheter slips out or the pump fails, you might not get the insulin you need and over time your sugars can increase and you could develop a dangerous complication called diabetic ketoacidosis. • Cost. Pumps are costly and so also are the infusion tubing and reservoir. Some of the new ones come with inbuilt sensors as well which are costly. Insurance companies do not approve of this usually. • The infusion tubing and reservoir have to changed once every three days • Sometimes the tubing gets kinked without delivering the insulin which could cause problems • One has to feed in the carbohydrate consumption at the start to prime the pump. • The insulin will not be delivered if there is air in the tubing or if the insulin remaining in the cartridge is very low. Jet Injector Jet injectors don’t have a needle. Instead, they use very high pressure to push a fine spray of insulin through the pores in your skin. Pros: • Needle-free. If you hate needles, a jet injector is an alternative to the insulin syringe or pen. Cons: • Pain. Though needle less, they can cause more pain in some of those with sensitive skin as the insulin is driven inside the body by sheer force. You have a high concentration of nerves close to the surface of your skin. Trying to push insulin through the skin can hurt more than injecting — especially considering how thin needles are. • Uneven insulin delivery. Because they send insulin into the body through the pores, jet injectors may not always deliver an accurate dose. Other options include an insulin patch. Work closely with your doctor to choose the option that best fits your budget, health needs, and lifestyle. Not all the above are available here in Oman. Afreeza is a powder form of insulin which is an ultra rapid acting insulin. The powder is used by an inhaler called the Dreamboat inhaler. Peak levels are reported in 12-14 minutes of inhalation. This is especially beneficial for those with type 1 diabetes who are dependent on insulin for life and also for those with type 2 who become insulin dependent with failure of the pancreas. Close to 5300 patients have been studied in trails across the world and the results so far are promising, but needs further time to be found effective. This has been found to reduce the post meal sugar levels, fasting levels, have less incidence of hypoglycemia( term used for low sugar levels) , reduced weight gain as when compared to rapid acting insulin. However, this may need to be combined with long acting insulin or with oral medicines as the case may be for a better effect. The side effect so far noted has been a non productive cough ( dry cough) Degludec insulin is a new ultra long acting insulin which is still on research programs to test its efficacy. Though it is being marketed for injection once in 3 days or once a week ( which sounds like sweet music) , the effects of the insulin wear off after a day or two. Which means it is still better to have the shots of insulin daily for better control. The sugar control and episodes of low sugar have not shown any improvement over the insulin preparations available in the market today. Continuous glucose monitoring 
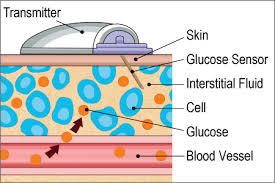 Continuous Glucose monitoring (CGM) devices are in the market for quite some time. These are small gadgets the size of a pager which help to monitor the sugar levels throughout the day and night. On an average a child between the ages 5 and 14 may have to poke the finger for sugar checking at least 50000 times and about 15000 injections of insulin during that time. This is quite phenomenal and frightening. For people on intensive insulin therapy as among those with type 1 diabetes or among those with frequent dips or spikes in their sugar levels which could be related to either food, alcohol or exercise. These machines detect the glucose level just under skin with the help of sensors. These levels are transmitted to a receiver. Pros: • This will give a constant reading and you can adjust the doses accordingly with the help of the health care provider. If the blood glucose reading is 7 mmol/L or 126 mg/dL, it could mean the sugar is going up or down and that is the reading at that time. The machine gives an arrow mark which will give the trend based on the readings just before.. • The tracings can be downloaded and interpreted • The tracings are given for every day in different color lines for easy interpretation • It also gives the average and how many lows one had experienced in the interim. • Alarms are there which could be programmed into the machine which could go on either when sugar swings too low or too high. Cons: • The cost is quite high • Normally the insurance companies do not approve of this unless in certain cases. • The sensors will have to be changed once in 3-7 days. This is costly • This is to be worn at all times. • May not be feasible for children below the age of 12. • One will have to calibrate the machine from time to time so that the readings are accurate. Needle less devices Frequent puncturing of the delicate skin at finger tips and also the insulin shots which are so frequent especially among those with type 1 diabetes are a cause of frustration. Now-a-days needle free CGM devices are coming out. Some are awaiting patents. There will be sensors, a transmitter and receiver. The signals can be sent to smart phones, computers or even laptops. This can be useful for working mothers who have children at home and can remotely access the sugar levels and send information to make corrective steps. The sensors are to be changed once in 3 days which helps prevent skin irritation. The skin top layer which comprises dead cells is painlessly removed and leaves a small abrasion not visible to the naked eye. The Symphony is one brand making such needle free CGM. Dexcom G4 Platinum is awaiting patents rights. This is sleek and hardly noticeable
Continuous Glucose monitoring (CGM) devices are in the market for quite some time. These are small gadgets the size of a pager which help to monitor the sugar levels throughout the day and night. On an average a child between the ages 5 and 14 may have to poke the finger for sugar checking at least 50000 times and about 15000 injections of insulin during that time. This is quite phenomenal and frightening. For people on intensive insulin therapy as among those with type 1 diabetes or among those with frequent dips or spikes in their sugar levels which could be related to either food, alcohol or exercise. These machines detect the glucose level just under skin with the help of sensors. These levels are transmitted to a receiver. Pros: • This will give a constant reading and you can adjust the doses accordingly with the help of the health care provider. If the blood glucose reading is 7 mmol/L or 126 mg/dL, it could mean the sugar is going up or down and that is the reading at that time. The machine gives an arrow mark which will give the trend based on the readings just before.. • The tracings can be downloaded and interpreted • The tracings are given for every day in different color lines for easy interpretation • It also gives the average and how many lows one had experienced in the interim. • Alarms are there which could be programmed into the machine which could go on either when sugar swings too low or too high. Cons: • The cost is quite high • Normally the insurance companies do not approve of this unless in certain cases. • The sensors will have to be changed once in 3-7 days. This is costly • This is to be worn at all times. • May not be feasible for children below the age of 12. • One will have to calibrate the machine from time to time so that the readings are accurate. Needle less devices Frequent puncturing of the delicate skin at finger tips and also the insulin shots which are so frequent especially among those with type 1 diabetes are a cause of frustration. Now-a-days needle free CGM devices are coming out. Some are awaiting patents. There will be sensors, a transmitter and receiver. The signals can be sent to smart phones, computers or even laptops. This can be useful for working mothers who have children at home and can remotely access the sugar levels and send information to make corrective steps. The sensors are to be changed once in 3 days which helps prevent skin irritation. The skin top layer which comprises dead cells is painlessly removed and leaves a small abrasion not visible to the naked eye. The Symphony is one brand making such needle free CGM. Dexcom G4 Platinum is awaiting patents rights. This is sleek and hardly noticeable












